
5 min read
Considerations for Critical Care Leader Rounding
Nobl Health Apr 21, 2020 1:11:00 PM
The admission of a loved one into a critical care area can put a family into “crisis” mode, especially when a hospital stay is unexpected. Until the status of the patient is known, the priorities for the patient and family revolve around two areas – information and support. Family members at the bedside are often tasked to keep the extended family and friends informed about the situation or to field multiple calls from those with well-meaning intentions. This is not a time to ask the family how your team is doing. The priorities of the nurse leader should be to listen and observe for ways to meet the needs of the family. Who are the members of their “team” and what level of information will be needed for each of them? How can you see the situation through the eyes of those waiting? What would you want if it was your loved one in critical condition? The opportunity to make a personal connection to the patient “through the lens of their family” will create a true patient-driven experience. We always hope for “happy endings” for our patients, but not all critical situations end with healing. A personal connection between the leader and the family/visitors can contribute to coping and healthy grieving.
What time is appropriate to round in critical care units?

To patients and families in the ICU, days and nights are much the same, with hourly assessments, medications and other life-saving treatments around the clock. It is no wonder that one in every three patients with an extended critical care stay will develop some form of ICU psychosis.1 For the family members (often sleeping at the bedside) it is hard enough to see their loved one going through physical challenges, but it is even more stressful when Dad starts to become aggressive or see things that aren’t in the room. Individual patient and family needs often make it difficult to find the ideal time for nurse leader rounds. As much as we may want to schedule our day to complete expected rounds, rounding times must be at the convenience of the patient/family and the healthcare team. Routine participation of nursing leaders in interprofessional clinical rounds can identify anticipated concerns and reveal when and who a leader should approach for a leader round. By knowing the plan of care, a nurse leader can manage up the team and build trust by providing information that is consistent with what others are saying.
Another way to connect with family of the critically ill patient is to ask them when they plan to visit or what time seems convenient for them. Years ago, I was the primary care partner for my elderly mother and journeyed through five critical care admissions over an 18-month period before we made the decision to head into hospice/homecare. She had excellent care on each visit and was treated with respect and concern, but not once was I asked if there was a good time for leaders or providers to come to check in with me. Respecting the care partner need for ongoing information and support is critical.
Even with thorough preplanning, there will still be times when rounding on the patient or family is not possible.
What are expectations for rounding when patients cannot personally respond?

When the patient is too ill to respond, and care partners are not available, is there even a reason to attempt a round on the room? There is always value from a leader visit to a patient room. Performing an environmental assessment or safety round, can proactively detect issues before they become emergencies. Compliance with policies or practices such as white board completion, bed alarm usage, IV tubing labeling, or infection prevention protocols can be assessed without disturbing the patient. It also provides the opportunity for the leader to see the care area through the eyes of patient, family, or other visitors. For those of us who have spent our entire careers in healthcare, the work becomes routine. It often takes an external cue to raise our consciousness on behalf of those who are not familiar with the routines, jargon, and equipment in hospitals. Leader rounding is that cue and setting goals to hold everyone accountable is a plus.
In addition to environmental rounds, Nobl clients also have the option to count “rounding attempts” as a completed round when multiple stops at the bedside don’t result in a completed visit. Using this as an option can “fill a square” so critical care leaders can meet established leader rounding goals and accountabilities. But the best option might be to create customized unit-level nurse leader goals that encourage purposeful activities rather than just meet safety and patient experience goals.
How do we set realistic rounding goals when “few” patients can respond?

Setting realistic and attainable nurse leader rounding goals is not an easy task. In smaller community hospitals, nursing leaders often have accountability for multiple care areas or additional processes/projects. In large academic medical centers, large units may have dozens of critical care beds in multiple pods or hallways. The best goal-setting approach is based on these easy steps:
-
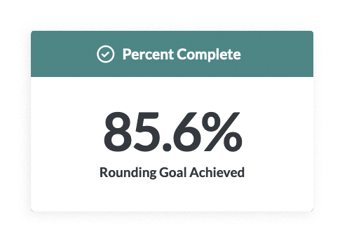
Round on responsive patients every day; round on family or visitors who are present daily or every other day, as available; perform an environmental assessment as indicated by the findings or previous rounds. Averaging these expectations, an initial rounding goal can be determined. At Nobl we see a positive correlation between rounding and outcomes when compliance ranges between 65 – 80%.
-
Evaluate the unit census to determine the average number of patients a) who can respond and engage within a patient round, b) have visitors or family available for a round, and c) how often environmental or safety check rounds are really needed. Based on that number, use a rounding formula to determine a realistic rounding goal for each type of leader round.
-
The final expectation is that rounds on alert patients and family are met and environmental assessments are completed to assure safety and comfort. When ANMs or unassigned charge nurses are available, the task to perform the environmental assessment/safety round on nonresponsive patients with no family present might be delegated to them.
Thoughtfully evaluate realistic goals and really discuss what is to be achieved. When rounding becomes a “check-box” exercise, it is not a good use of valuable leader time and doesn’t achieve the outcomes desired.
What are other ways to engage visitors and family when the patient is critically ill?

It is clear from this discussion that at times the leader will not be in a position to round, and at other times the patient and family may not be able to accept or value a visit. There are other ways to engage and make sure that patients/families feel valued by nursing leadership.
- Leave a nurse leader calling card and personal message for the family
- Provide family question/comment cards and a place to leave them for the leader
- Set up a nurse leader “hotline” to capture family/visitor concerns
- Create “patient storyboards” to mark patient milestones and accomplishments (useful to help acutely ill patients capture “time lost” later when they are recovering)
Maximizing Use of the Friends and Family Portal in the Critical Care Setting

The Friends and Family Portal™ is a feature unique to the Nobl Rounding Platform. The portal makes it easy for others to check on the patient securely over any internet connection when they can’t be at the hospital. Critical care units can customize icons to communicate the typical needs of their population to add optimal value to the product. Reinforcing the availability of the portal, what information it contains, and how to use it is an important part of a leader round. Rounding on visitors can provide valuable information based on their observations, ideas, and needs as well as their use and satisfaction with the portal. When completing post-discharge satisfaction surveys, patients are often influenced by the perceptions of family members, so this is an important population to keep in mind.

The culture and characteristics of a critical care unit are defined by the physical layout, provider and staff values/practices, and patient/family needs. Each critical care unit is a special and separate use case. It is very important to plan leader rounding that accounts for leader availability and workload, patient and family needs, and the overall purpose and desired outcomes of rounding. Just “filling squares” is a wasted opportunity.
Written by Teresa Anderson, EdD,MSN, NE-BC, Nobl CNO
1 Shiel, W. (2008). Medical Definition of Intensive care unit psychosis. Downloaded January 3, 2020 from https://www.medicinenet.com/script/main/art.asp?articlekey=6882
New Free eBook
Best Practices for Sharing and Reviewing Data from the Nobl Rounding Platform
Beryl Institute Case study
Improved First Impressions at Your Front Door - Patient Ambassador Rounders Enhance the Patient Experience of a Busy Emergency Department
Recent Posts

Staffing Issues Shouldn’t Derail Patient Rounds



